Standard Machine-Readable File Recommendations for Hospitals
Standard Machine-Readable File Recommendations for Hospitals
The CY22 proposed rule covered many topics, but, in our opinion, the guidelines and clarifications surrounding machine-readable files were some of the most critical.
The Proposed Rule’s observation that there was a “lack of uniformity in the way that hospitals display their standard charges (84 FR 65556)” wasn’t a great surprise to the industry. The original guidelines required certain data elements but did not specify an exact file structure. Hospitals naturally constructed a file that best fit their data, but these files could be difficult to compare from one hospital to the next.
CMS has been very clear that its goal is to make the data as accessible to the public as possible, so it’s understandable that they saw clarification in this area as a priority. We believe CMS is right that there is a wide variety of file structures out there, and that makes it hard to meaningfully compare hospitals. Our research shows a few challenges to fixing this particular issue.
First is the presence/updates of information. How do we locate and download the files? This issue will improve once hospitals use the CMS naming convention for machine-readable files. Another solution would be for CMS to define “prominently displayed” as requiring two clicks from the hospital or health system home page.
The next challenge is file type and layout difference. There’s a lot of variation between hospitals and systems. Requiring the same file type and standardizing the structure, as well as defining the data elements, could resolve this and will help create a national database.
Relational differences are another hurdle. Hospitals sometimes report payer-specific negotiated charges with HCPCS, MS-DRG, APC, per diems, case rates, and charge codes. This variation can be solved by creating a standardized display.
Payer naming differences also cause issues since there are no standardized naming conventions. Again, a uniform structure can solve this issue.
To this end, we have constructed a proposed standardized single machine-readable file. In December 2019, CMS stated that a single machine-readable file could have different sections but needed to contain all required elements. Here’s how each section could be defined to allow for uniform reporting. What follows is a summary of our recommendations. You can find a more detailed description here.
Section One: Gross Charge Information
This includes six fields. The primary comparison link is CPT®/HCPCS; revenue codes can also be compared on a more manual basis through item descriptions, as well (useful for room rates and operating room associated codes, as primary examples).

Section Two: Discount Cash Price Information
Not all hospitals have established their cash pay policies in the same way. To account for this variation while still permitting standardized reporting, we believe the “Discount cash price” section should have two options, Policy and Price List.
Policy – a text field for an explanation of the hospital’s policy, how it is applied, and contact information for financial assistance.
Price List – for hospitals with an established price list, information could be displayed in the same format as the Gross Charge display.


Section Three: Payer-Specific Negotiated Charge
This is the area that contributes most to the lack of consistency within the files. There is an incredible amount of variability. It is very difficult to compare payers and plans from one hospital to another. Here is how we propose tackling it.
Standardized Payment – Unless all payers utilize the same payment methodologies it isn’t possible to look at payment differences. Standardized payment rates and utilization must be considered in order to understand payment differences. CMS has established payment systems for inpatient and outpatient claims that are utilized by all hospitals subject to the transparency reporting requirements. The solution to standardizing disparate payment systems is for hospitals to determine how the claim would be paid using the specific payer negotiated contractual language and then reported under Medicare-based grouping logic by MS-DRG (inpatient) or primary APC (outpatient). The steps to do this, are:
- Derive expected claim payment for all items and services based by consulting the negotiated rates and terms with the specific payers. This would be done for all claims – not using historical reimbursement – but a calculation of payment using current payment terms and rates.
- Determine the MS-DRG (inpatient) or primary APC (outpatient) assignment for the particular patient claim. Grouper logic is quite common for hospitals and many already run every claim through Medicare logic to determine a MS-DRG assignment. Each claim would be labeled with a MS-DRG or primary APC designation (more on outpatient grouping later).
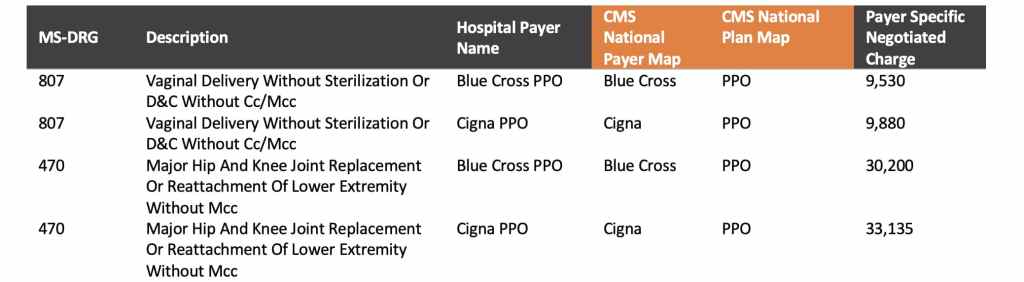
- Report the standardized payer-specific negotiated charge by MS-DRG or APC for all required payers in a simple format illustrated below. This display would encompass all items and services and service packages and would also be representative of service utilization – the critical element needed to understand payment differences.
Again, further details can be found here. Hospitals could derive the payer-specific negotiated charges with their contracted rate sheets and terms and applying those to actual patient claims. Without patient claim detail the hospital cannot satisfy the requirements of the rule because the number of combinations of items, services, and service packages is nearly limitless on a per-patient basis.
Standardized Payer Mapping – Once payment has been standardized, payers must be compared through common mapping. CMS could create a list of national/regional payers and the hospitals could link to that. This map could be for the top twenty or thirty payers and would allow for easier comparisons.
Standardized Reporting Structure – Here is a simple, standardized format that would accommodate these needs.

Section Four: Payer-Specific Negotiated Charge
The benefit of using the structure identified in Section Three is that minimum/maximum values are very easy to present. A researcher could easily calculate minimum, maximum, and other statistical measures based on the standardized data format presented. Still, this information could be compiled like this:

We believe that if the CMS seeks to standardize the Machine-Readable File it should do so in a way that will meet current requirements while providing meaningful information. The structure we have proposed addresses these requirements and solves for the challenges that stakeholders are experiencing with current disclosed data.
To see a complete summary of the proposed rule, click here! To see our complete response, click here!
To watch our free summit on Price Transparency, check it out here!
- 1
- 2
Comments (0)